Rotator Cuff
The rotator cuff corresponds to a musculo-tendinous complex that surrounds and covers the joint between the humerus and the scapula. This essential structure allows shoulder mobility but can be subject to lesions requiring specialized management.
Definition
Rotator cuff rupture = detachment/tear of the tendon from its attachment to the bone
Causes
- Traumatic (fall, dislocation)
- Progressive wear (subacromial bone conflict)
Examination
Arthro-CT or arthro-MRI (reference examination)
Surgical treatment
- Arthroscopy
- Hospitalization: 0 to 2 days
- Under general anesthesia
- Immobilization: 45 days (abduction pillow)
- Physiotherapy: 5-6 months
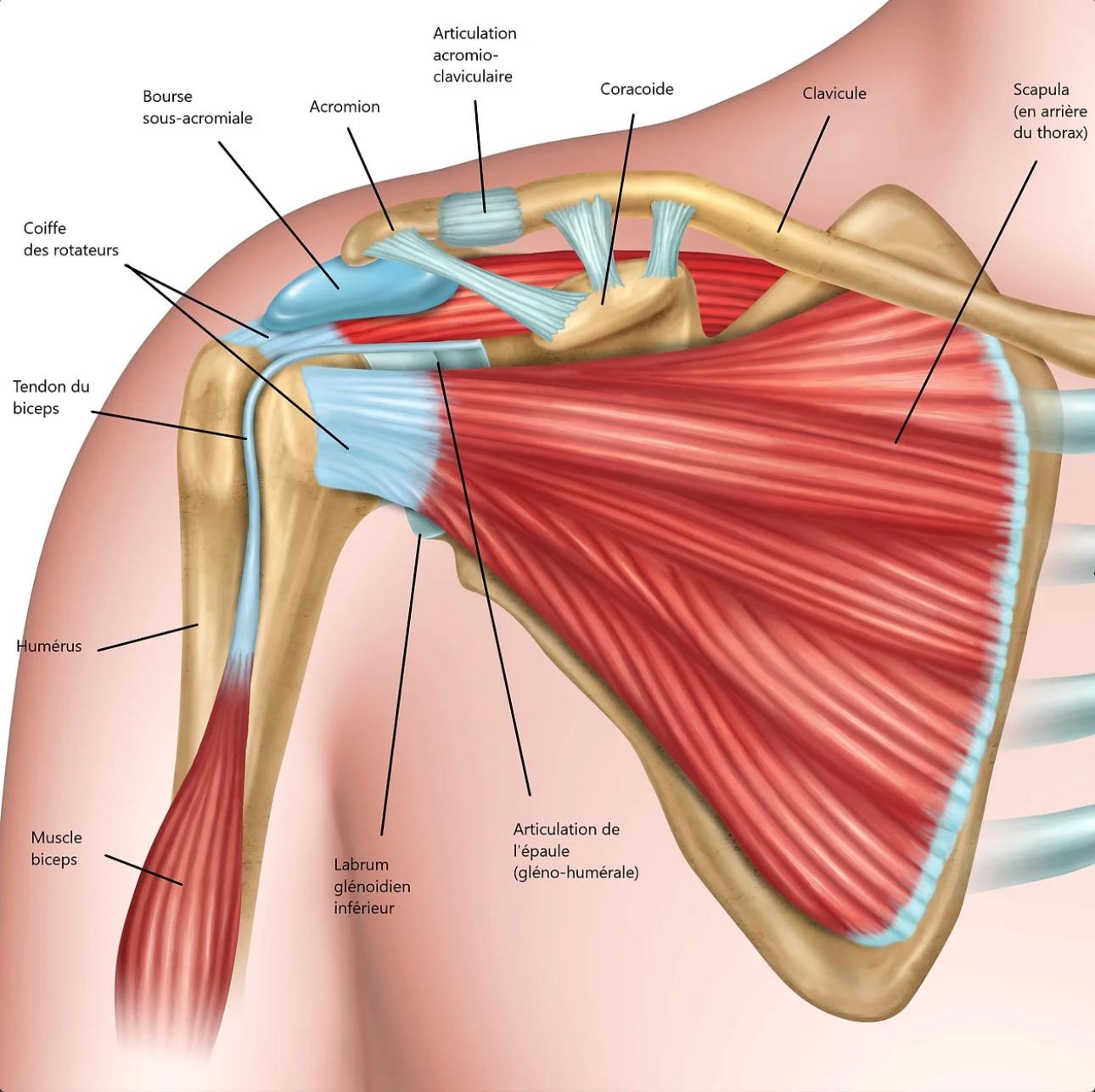
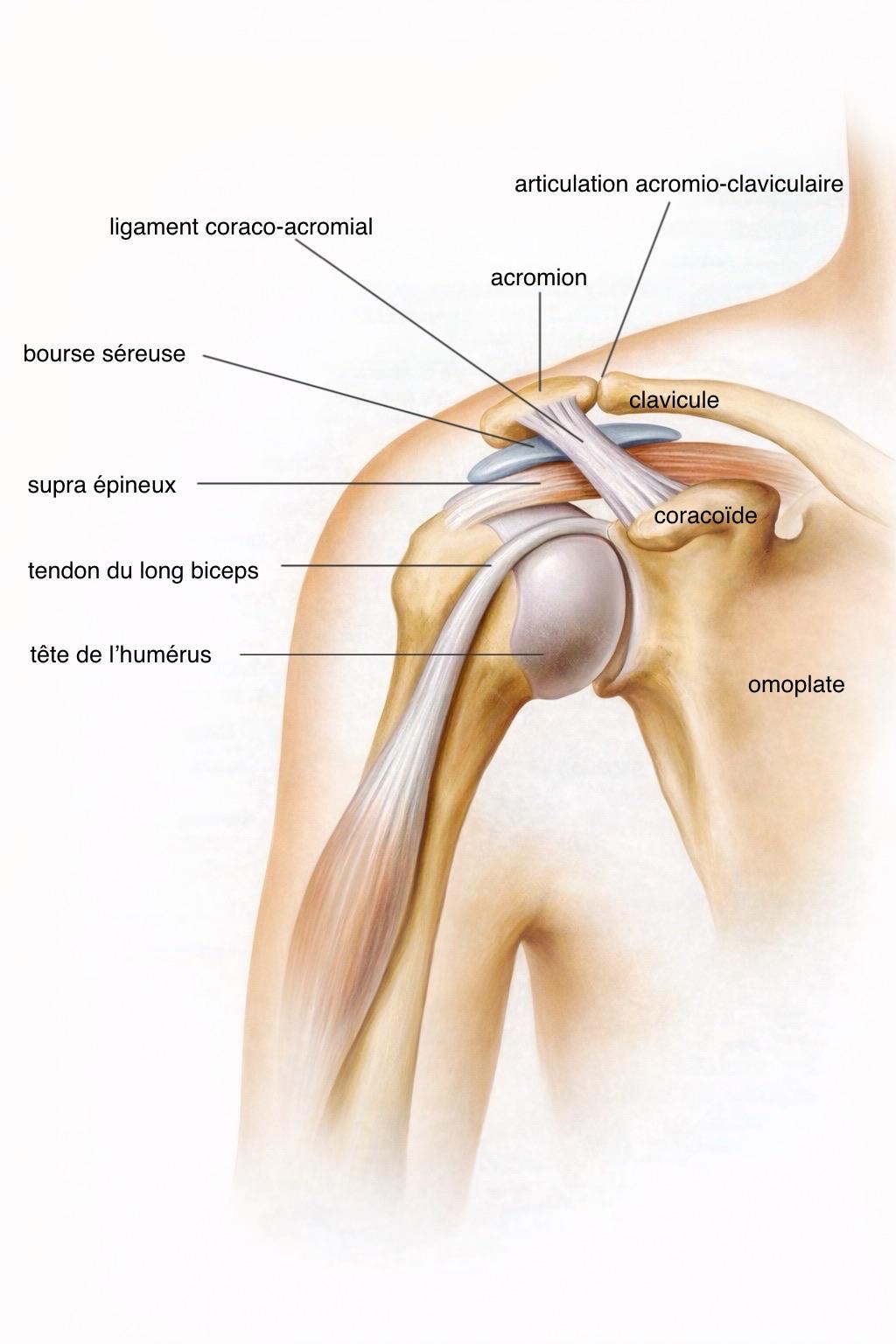
The rotator cuff corresponds to a musculo-tendinous complex that surrounds and covers the joint between the humerus and the scapula. This musculo-tendinous cap hermetically closes the glenohumeral joint in physiological conditions.
The cuff is composed of four tendons that attach to the humeral head, allowing the different movements of the shoulder and arm in all directions of space. It is thanks to it that the shoulder joint is the most mobile in the human body.
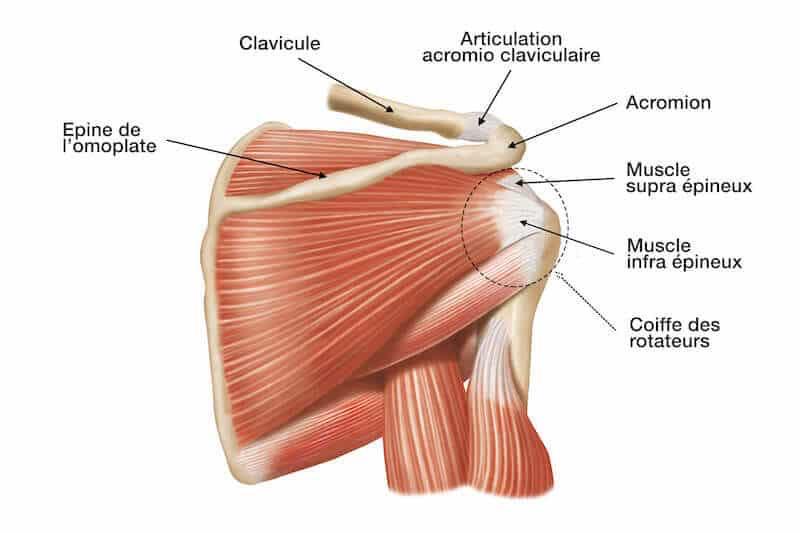
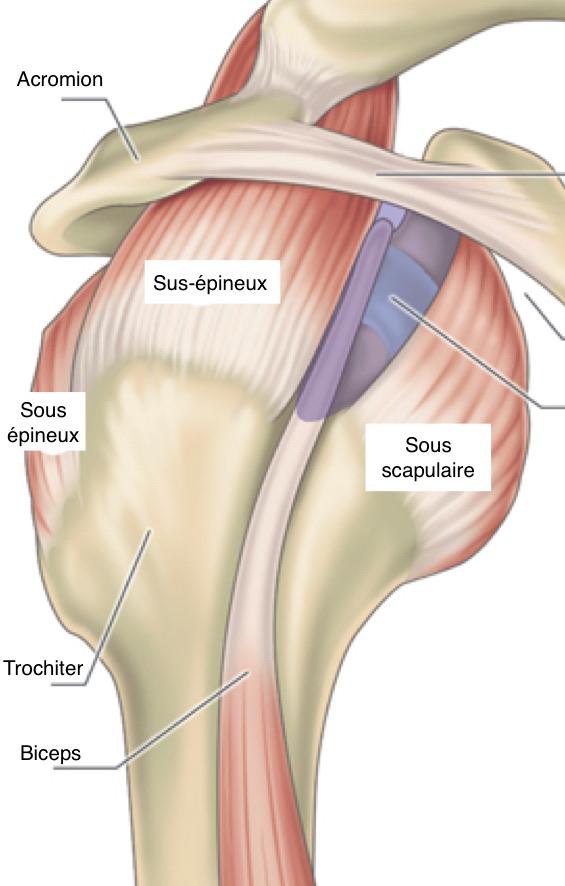
The rotator cuff is composed of four tendons that attach to the humeral head:
- Subscapularis (anterior): attaches to the lesser tuberosity of the humerus
- Supraspinatus (superior): inserts on the greater tuberosity of the humerus at its superior part
- Infraspinatus (posterior): inserts on the greater tuberosity of the humerus at its superior part
- Teres minor (posterior): inserts at the posterior and lateral part of the humerus
Rotator cuff lesion: This is an alteration or intrinsic injury to the tendon structure, to its attachment to the bone at the humeral head level (at the greater or lesser tuberosity).
The tendons of the rotator cuff allow the different movements of the shoulder and arm in all directions of space:
- Anterior elevation movements
- Lateral elevation movements (abduction)
- Internal or external rotation movements
This great mobility will also be at the origin of the fragility of these different structures and in particular of the rotator cuff.
Crack/Rupture
Tendon injury can occur along the axis of the tendon fibers, in which case we speak of a tendon crack. The lesion being parallel to the tendon fibers, the functional impact is often less significant.
It can also be perpendicular to the tendon fibers and in this case we speak of a rupture or detachment of the tendon from its bony attachment. Since this is a complete detachment of the tendon, the functional impact is often much more significant.
Partial/Total
The tendon lesion may affect only part of the tendon thickness, in which case we speak of a partial lesion of the rotator cuff affecting either the deep part of the tendon on the articular side, or the superficial part of the tendon on the extra-articular part.
In case of a lesion affecting the entire thickness of the tendon, we speak of a transfixing lesion, meaning that the lesion completely penetrates the tendon from side to side.
One or several tendons
The rotator cuff lesion may affect only one tendon in isolation: it is the supraspinatus tendon that is affected in more than 80% of cases.
It can also affect several tendons at the same time or even all simultaneously in case of complete rotator cuff rupture.
There are 2 main reasons for tendon injury: degenerative causes and traumatic causes.
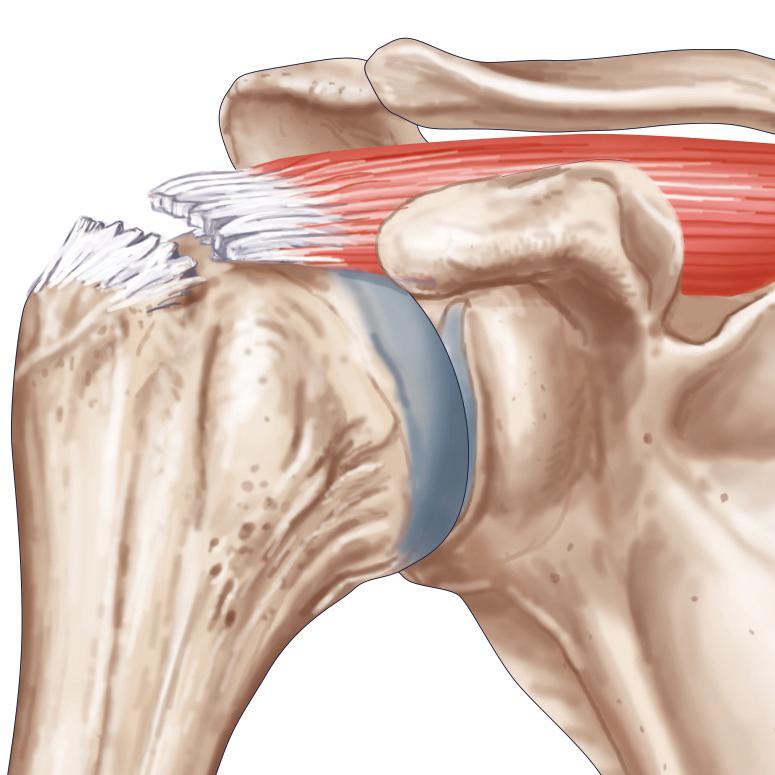
Subacromial impingement
It is the repeated friction of the different tendons of the shoulder against the acromial bone (+/- aggressive) that will cause progressive weakening of the rotator cuff.
The evolution of this friction will cause a tendon lesion, which can range from superficial partial lesion to complete rupture. This complete rupture can occur either spontaneously or following a minimal effort or a fall.
There is often a context of chronic shoulder pain dating back several months or years with a history of bursitis or shoulder tendinitis.
Sometimes, a more or less intense triggering factor is found such as carrying loads, a constrained movement or a fall, which will complete the rupture.
Upper limb trauma
Traumatic rupture of the rotator cuff most often occurs in the context of a fall. It can be a fall directly on the shoulder stump, on the elbow or even the arm forward.
It can also be direct trauma in the context of heavy objects falling on the shoulder stump or percussion, particularly during road traffic accidents.
Finally, shoulder dislocations are also responsible for sometimes massive lesions of the rotator cuff tendons. Indeed, during glenohumeral dislocations, the humeral head leaves its physiological position causing significant traction on the tendon attachments and a major risk of tearing.
This risk of tearing increases with the age of patients due to greater tendon fragility, most often after 50 years.
Rotator cuff rupture corresponds to a tearing of the tendon from its attachment at the bone level (humeral head). This rupture will most often manifest as severe pain, accompanied by functional impairment and sometimes a pseudoparalytic shoulder.
During the trauma or false movement, the patient often feels a sensation of snapping or tearing.
A few days or weeks after the accident, the painful phenomena as well as inflammation decrease, giving way to more or less significant functional impairment as well as lack of strength.
Pain
They are often very important during the acute phase at the time of trauma with sensation of cracking or tearing (clearly described by the patient).
These pains will be constant throughout the day, without real fluctuation between day and night, unlike inflammatory pains.
It is immobilization and rest, with the arm in elbow-to-body position, that will best calm these painful phenomena.
After several days or weeks, the pains calm down and may disappear completely, or give way to inflammatory-type pains.
In case of underlying chronic subacromial impingement, the pains may disappear very quickly after the rupture.
In case of traumatic rupture, the evolution can often be complicated by retractile capsulitis phenomena (frozen shoulder picture).
Topography
Pains are most often located at the shoulder stump, at the anterior and lateral part.
In the acute phase, it is sometimes possible to precisely describe the painful area corresponding to the torn tendon area. They are very regularly located at the anterior and lateral part in front of the biceps tendon but also in superolateral in front of the supraspinatus tendon.
After a few days, the pains are often more diffuse and less systematized due to reactive inflammation and possible associated muscle contractures.
Irradiation
Pains radiate relatively little during the acute phase but most often after a few days of evolution.
The pains will therefore move with irradiation most often in the arm along the long portion of the biceps but also up to the elbow or even the wrist.
There may also be reactive muscle contractures to the rupture causing pains in the muscle compartments, whether dorsal (latissimus dorsi muscle), cervical (trapezius muscle) but also anterior in front of the pectoralis minor.
Triggering phenomenon
Mobilization of the arm and shoulder, particularly on elevation or rotation movements, will induce more or less significant painful phenomena, particularly during the acute phase.
Vibrations, particularly during car journeys, can also trigger the pains, as can shocks or false movements on the affected arm.
Note that pains are very variable from one person to another, particularly in terms of intensity. Therefore, a total absence of painful phenomena does not necessarily exclude a rotator cuff tendon rupture.
Functional impairment
Functional impairment corresponds to the inability to normally mobilize the affected limb.
Just like pains, functional impairment is very variable from one individual to another. The importance of functional involvement will not necessarily be correlated with the importance of the tendon lesion.
Functional impairment will most often manifest as a lack of strength, more or less significant or even total, during movements related to the affected tendons.
For example, in case of supraspinatus tendon involvement, a lack of strength will be found during anterior and lateral elevation of the arm.
In some cases of massive rotator cuff lesion (involvement of several tendons), there may be a pseudoparalytic shoulder picture corresponding to a total inability to actively mobilize the arm.
Note that in case of isolated cuff lesion, arm mobilization remains preserved, the deficit only concerns active mobilization.
After several days or weeks, it is possible that other undamaged tendons and muscle structures take over from the torn tendon. The patient can in this case recover a more or less complete active mobility of the arm but there most often persists a lack of strength in movements related to the torn tendon.
Attention: recovery of shoulder mobility following a rotator cuff tear does not mean that there has been healing or repair of the damaged tendon.
Contractures/capsulitis/joint stiffness
It is frequent in the aftermath of a rotator cuff rupture, particularly in the context of traumatic ruptures, that stiffness phenomena appear during passive mobilization.
Indeed, in cases of traumatic rupture, bleeding occurs in the joint, promoting adhesions and tissue attachments. These different interarticular adhesions will cause limitation of joint amplitudes as well as stiffness.
The same applies during shoulder dislocation phenomena but also in case of prolonged immobilization after trauma.
It is also possible in the aftermath of a rotator cuff lesion that inflammatory signs appear affecting the joint capsule, which can also be the origin of significant stiffness and limitation of joint amplitudes.
These capsulitis phenomena are all the more frequent the longer the immobilization has been prolonged after a possible trauma.
Finally, in case of chronic painful phenomena, reflex muscle contractions aimed at analgesia can be the origin of muscle contractures maintaining the painful phenomena and shoulder decentering.
Clinical examination
The clinical examination will find signs of rotator cuff lesion allowing us to orient towards the injured tendon.
This examination will be more or less difficult to perform due to painful phenomena following the rupture.
In the immediate aftermath of tendon rupture, the clinical examination is most often not feasible due to painful phenomena. Active-passive mobilization of the shoulder is most often impossible and irritative signs are predominant.
After a few days of rest (10-15 days), the painful phenomena decrease significantly with recovery of passive mobility allowing the performance of a specific clinical examination.
It will therefore be possible to perform the specific rotator cuff tests to detect the affected tendons.
Many tests exist allowing us to orient more or less specifically towards the damaged tendon area:
- Jobe test: to demonstrate supraspinatus tendon involvement (or its variants: empty can test, full can test, champagne toast position)
- Belly press test, Lift off test, Bear-hug test: to demonstrate subscapularis tendon involvement depending on the affected tendon area
- Patte test: to evaluate the infraspinatus
Note also that in case of inflammatory phenomenon or joint stiffness, these tests can be falsified or poorly interpretable.
Paraclinical and complementary examinations
Standard X-ray: frontal and profile
This is the first routine examination to perform in case of shoulder pain, it will provide much information on the different bone structures of the shoulder.
It does not allow direct visualization of the rotator cuff or soft tissues but on the other hand allows detection of many indirect signs of rotator cuff rupture.
In case of trauma, it will also allow searching for bone lesions or possible fractures.
The frontal X-ray allows to judge:
- Distance between the acromion and the humeral head, allows to judge the centering or possible elevation of the humeral head relative to the glenoid (elevation of the humeral head in case of rotator cuff rupture)
- Shape of the acromion, more or less aggressive character
- Shape of the acromioclavicular joint, possible presence of arthropathy and inferior overflow
- Possible intra-tendinous calcification
- Possible glenohumeral osteoarthritis
The profile X-ray: It allows visualization of the acromion shape and classification according to types 1, 2 or 3.
Attention: an aggressive acromion shape on X-ray is not synonymous with subacromial impingement even if it increases its probability.
Standard shoulder X-ray only allows seeing bone structures and in no case tendon or ligament structures.
Ultrasound
This is a minimally invasive examination allowing exploration of the tendon and muscle structures of the shoulder.
This examination being very operator dependent, it has a relatively low diagnostic reliability.
Ultrasound will allow finding signs of tendinitis with rotator cuff tendon thickening or even erosion.
It will also allow searching for signs of subacromial bursitis, namely inflammation of the bursa physiologically present between the acromion and the rotator cuff.
Possible rotator cuff lesions will also be searched for, whether fissure, rupture or detachment.
These rotator cuff lesions are often the consequence of prolonged subacromial impingement or an added fall.
In the acute phase, just after the lesion, ultrasound will often find signs of hemarthrosis, i.e., bleeding in the joint related to tendon tearing.
This examination will also allow characterizing the rotator cuff rupture:
- Type of lesion: fissure, rupture, detachment
- Topography of the lesion, affected tendon
- Size of the rupture and transfixing character
- Retraction of the lesion
Ultrasound is therefore a good screening examination but has many limitations, particularly difficulty in evaluating possible muscle atrophy, fatty involution but also the different interarticular structures, particularly the glenoid labrum.
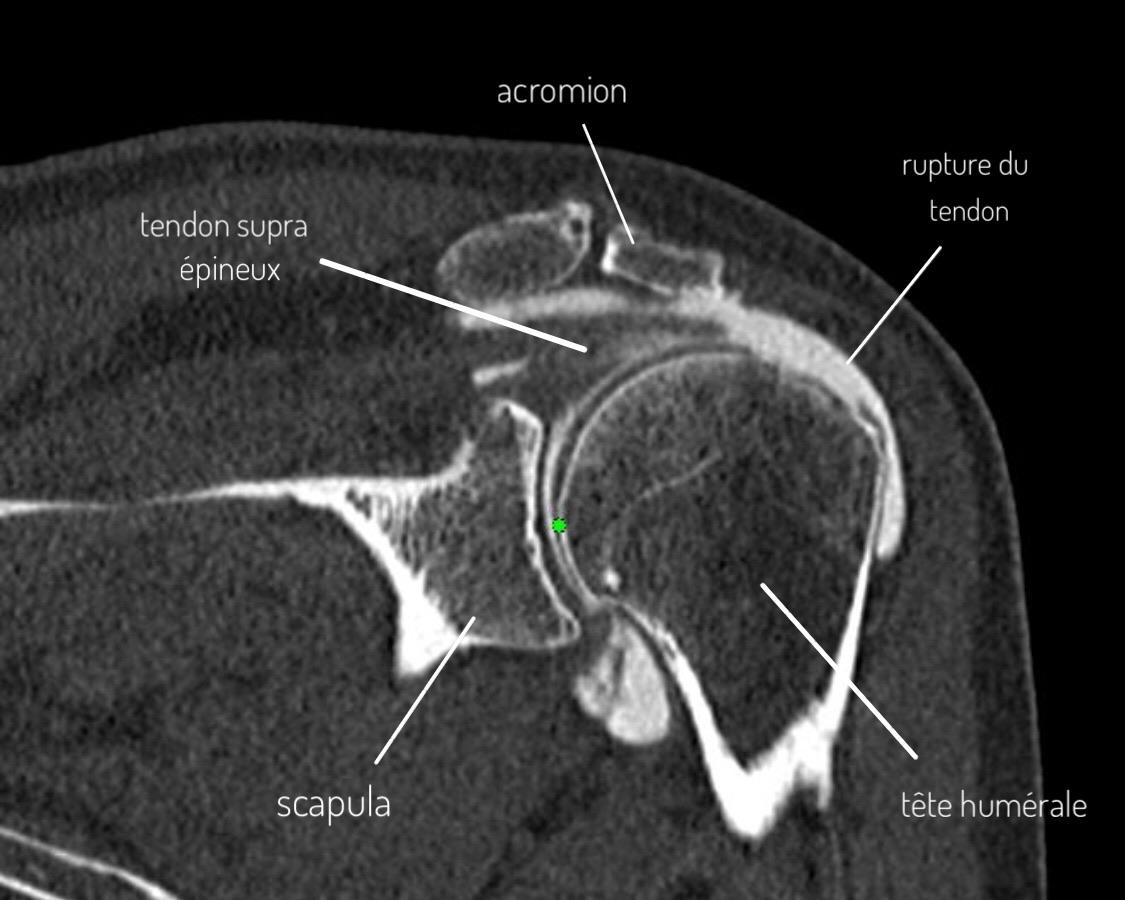
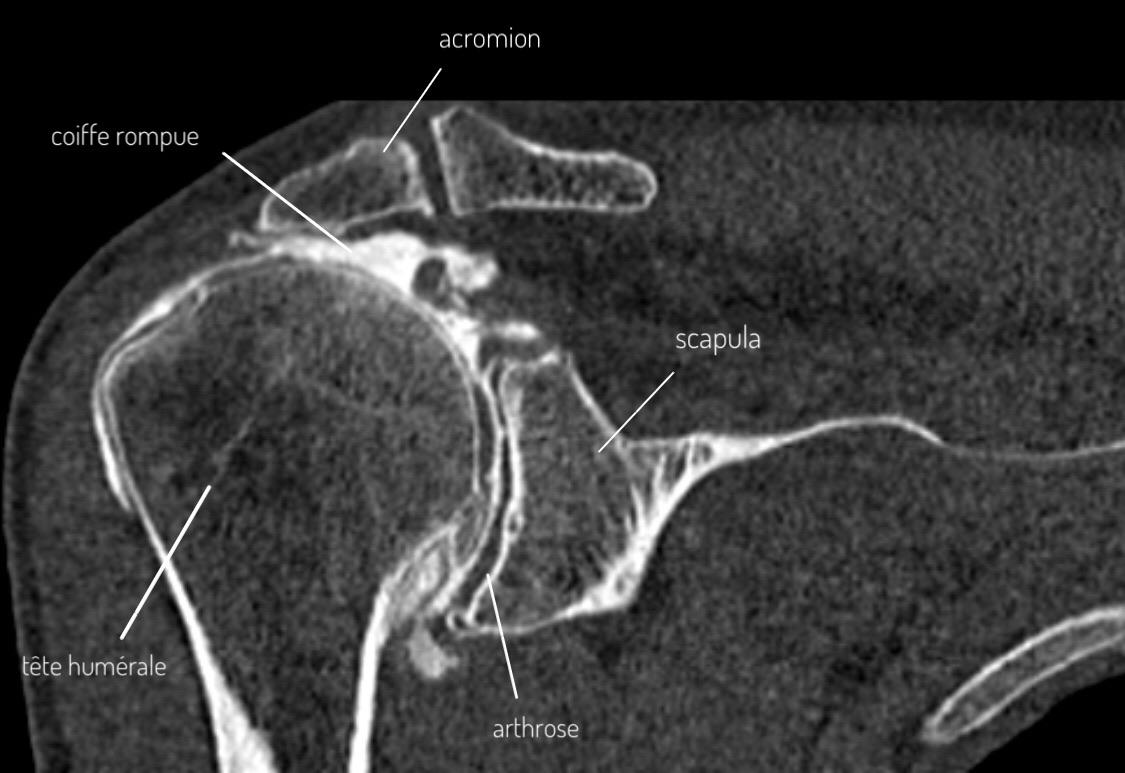
Arthro-MRI or arthro-CT: reference examination
This is the Gold Standard to confirm and assess a rotator cuff lesion, particularly in the context of preoperative assessment.
During this examination, a contrast agent injection is performed in the shoulder joint (between the humeral head and the scapula), followed by a CT scan or MRI.
The distribution of the contrast agent in the joint will allow perfect visualization of the different rotator cuff tendons as well as bone, cartilaginous and ligament structures.
This examination will therefore allow visualization of possible fissure or complete or incomplete rotator cuff rupture, consequence of prolonged subacromial impingement or fall.
It allows in particular:
- Precise visualization of the affected tendon(s) (supraspinatus/infraspinatus, subscapularis)
- Evaluation of lesion size (length and width)
- Evaluation of transfixing or non-transfixing character (affecting the entire tendon thickness or only partial)
- Evaluation of tendon retraction (stage 1, 2 or 3)
- Evaluation of muscle atrophy as well as fatty involution of muscle bodies (stage 0 to 4)
All these elements will allow defining the patient's operability criteria, particularly the technical possibility of reinserting the tendon in good position but also by muscle state to evaluate the subsequent functional character of the repair.
Other elements will also be visible during this examination:
- Signs of subacromial impingement with an aggressive acromion potentially at the origin of the lesion
- Signs of advanced osteoarthritis, particularly in cases of old rupture with arthrotic decompensation and humeral head decentering
- Signs of bursitis, hemarthrosis or associated capsulitis
It will also be possible at the same time as this examination to perform a cortisone infiltration to limit inflammatory or capsulitis phenomena, regain more comfort and joint flexibility.
This infiltration is not intended to cure a rotator cuff lesion but only to relieve painful and inflammatory phenomena. Its effectiveness is most often temporary.
Conservative treatment of rotator cuff lesions aims to reduce painful and inflammatory phenomena, and to promote functional recovery. It is particularly suited for patients with partial lesions or well-tolerated old ruptures.
Medication treatment
- Level 1 or 2 analgesics (rarely level 3): The choice of treatment will depend essentially on the intensity of pain but also on tolerance to different analgesics (paracetamol, tramadol, codeine...)
- Non-steroidal anti-inflammatory drugs: Treatment to be implemented for a duration of 5 to 10 days, with or without gastric protectors (PPI). Avoid prolonged treatment with anti-inflammatory drugs.
Immobilization
Shoulder immobilization is done with an orthopedic vest also called elbow-to-body sling.
This immobilization will be especially recommended in case of recent and traumatic rupture to promote healing and limit painful phenomena during the acute phase.
The recommended immobilization duration is generally 2 to 3 weeks in the acute phase.
Prolonged immobilization risks causing joint stiffness and retractile capsulitis phenomena.
Cryotherapy
Cryotherapy or icing corresponds to the application of cold in contact with the painful area several times a day.
It will have both an analgesic but also anti-inflammatory role, particularly during the acute post-traumatic phase.
It can be done at home with devices sold in pharmacies or more simply with bags of frozen peas (thus taking the shape of the shoulder).
In case of painful acute phase, it is recommended to apply icing at least 4 to 5 times a day for 15 to 20 minutes.
Cortisone infiltration
It corresponds to an injection of cortisone in the subacromial space or in the glenohumeral joint depending on the location of the lesion.
Ideally, this cortisone infiltration will be performed under fluoroscopic or ultrasound guidance to ensure proper needle positioning before injecting the product.
It is important to mention that this infiltration treats the symptoms and repercussions of the lesion but in no case the cause of it.
The infiltration can have very good effectiveness on painful and inflammatory phenomena, particularly in case of associated bursitis.
It will also allow regaining comfort and mobility to undertake physiotherapy in better conditions.
Its effectiveness is most often temporary and does not allow healing of a tendon rupture.
Note: Conservative treatment can be very effective for partial cuff lesions or well-tolerated old ruptures. However, it does not allow healing of a complete and transfixing rotator cuff rupture.
The choice of treatment is made on a case-by-case basis and will depend on many clinical and paraclinical factors.
The importance of tendon lesions but also physiology as well as the patient's age are important factors.
The degree of functional impairment, the age of the lesions but also the level of physical activity of the patient will be the main factors to consider in the choice of treatment.
Surgical indications
The choice of surgical treatment most often addresses young patients with important functional needs.
It will be particularly favored for active people, exercising a professional activity or regular sports activities.
However, there is no age limit for surgical management, physiological age being much more important than numerical age.
In the context of trauma at the origin of the rupture, management must be carried out quickly to avoid the occurrence of intra-articular adhesions but also the risk of significant tendon retraction which can make the intervention more delicate but also postoperative outcomes.
Overview of the surgical procedure
The principle of the surgical procedure is the repair/reinsertion of the torn tendon on its bony attachment at the humeral head level.
The procedure is performed under arthroscopy (video surgery) with 2 or 3 small incisions allowing insertion of a camera and surgical instruments.
Tendon repair is performed using anchors inserted into the bone, with double-row assemblies that represent the reference for obtaining the best stability.
For more details on the surgical procedure, see the Rotator Cuff Repair page.
The role of physiotherapy in the context of rotator cuff lesions is fundamental.
Acute phase
- Massages: muscle relaxation to avoid contractures
- Cryotherapy: analgesic and anti-inflammatory effect
- Gentle mobilization: decoaptation, relaxation and stretching
- Acupuncture, shock waves, electrotherapy...
Chronic phase
- Fight against shoulder elevation and anterior positioning
- Fight against muscle contractures
- Recovery of joint amplitudes
- Strengthening of healthy cuff tendons
- Functional work of the deltoid
After surgical intervention
Physiotherapy is fundamental after cuff repair. Duration: 5 to 6 months minimum.
Detailed program: Physiotherapy after Rotator Cuff Repair.
- Infection
- Bleeding/hematomas
- Tendon re-rupture
- Non-healing
- Nerve lesions
- Complex regional pain syndrome