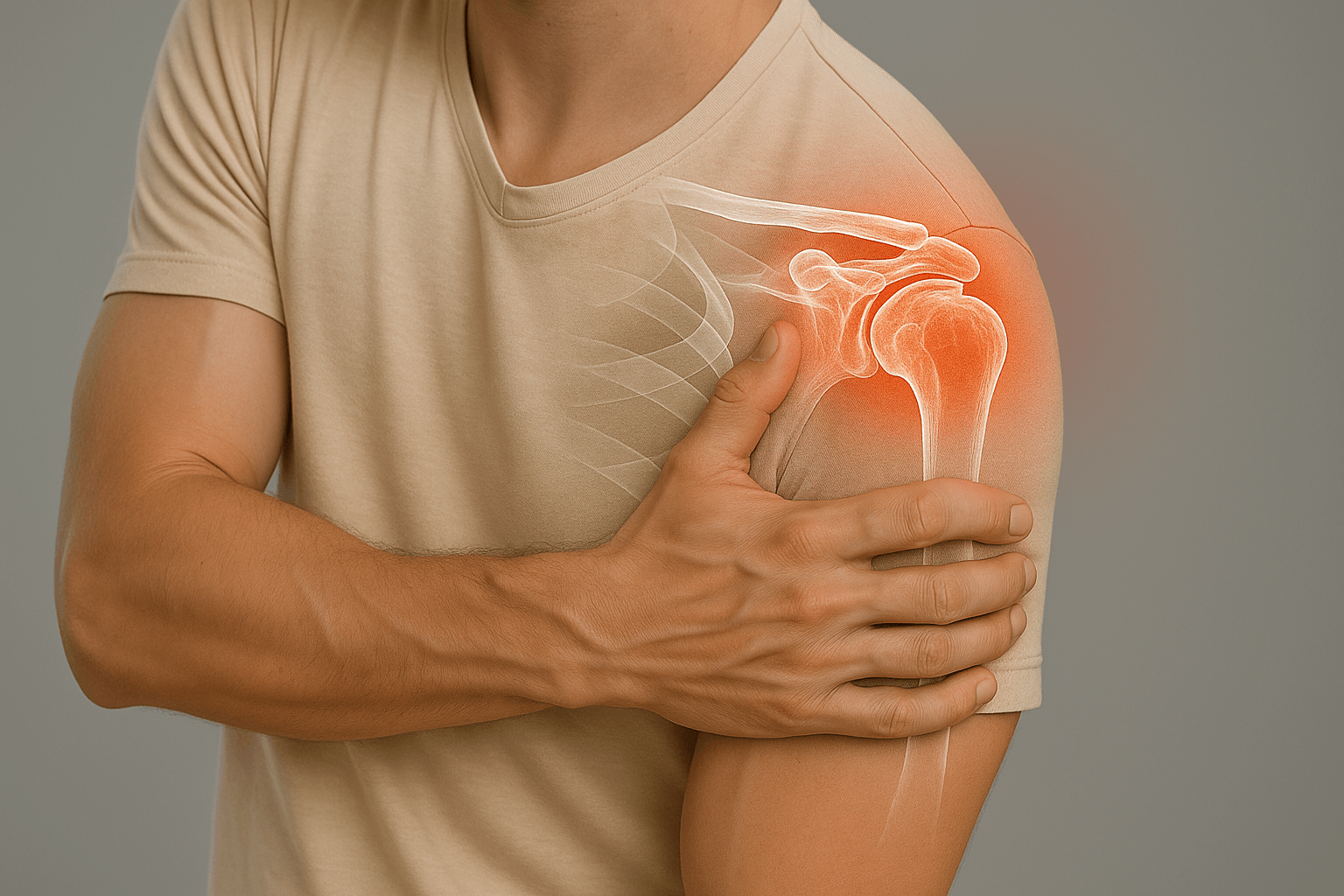
Shoulder Osteoarthritis (Omarthrosis)
Shoulder osteoarthritis corresponds to wear of the articular cartilaginous surfaces. This frequent pathology requires specialized management to optimize comfort and function.
Definition
Omarthrosis: wear of articular cartilage responsible for bone-on-bone friction
Causes
- Age, manual work
- History of fracture
- Repeated microtrauma
Clinical
Discomfort and functional impairment, pain +/-
Examination
Arthro-MRI or arthro-CT
Conservative treatment
- Little discomfort, little pain
- Physiotherapy and analgesics
- Infiltrations
Surgical treatment
- Open surgery
- General anesthesia
- Hospitalization 3 to 5 days
- Immobilization 45 days (splint)
- Physiotherapy 3 to 6 months
Definition: Osteoarthritis corresponds to an intra-articular lesion affecting the cartilaginous surfaces (humeral head and glenoid of the scapula in the case of omarthrosis).
Abrasion of the articular cartilage causes abnormal friction within the joint, progressively causing cartilage destruction.
In a healthy joint, the cartilage slides homogeneously between the two articular surfaces.
In case of osteoarthritis, it is the bone located under the cartilage that will rub against the bone on the other side of the joint (there is no longer cartilage allowing smooth sliding).
This abnormal bone-on-bone friction will induce joint remodeling in the form of geodes, osteophytes, joint deformation, free intra-articular fragments…
Physiology
The glenohumeral joint is the most mobile in the human body. Articular cartilage allows smooth and painless gliding between the humeral head and the glenoid of the scapula. In case of osteoarthritis, this function is altered, causing painful phenomena and functional limitation.
Bone-on-bone joint friction will cause joint remodeling with initially irritative and inflammatory phenomena going up to significant joint deformations. Clinical manifestations are dominated by painful phenomena but also stiffness or joint blockages.
Pain
In the context of shoulder osteoarthritis, painful phenomena are very fluctuating and very random.
Indeed, unlike lower limb joints (hip and knee), body weight does not rest on the shoulders, therefore constraints are less important and pains are often weaker and better tolerated.
There can therefore be very important and very advanced arthrotic phenomena associated with little pain or functional discomfort.
And conversely, very mild or moderate arthrotic phenomena associated with painful phenomena and major functional impact.
There can also be sensations of electrical discharges or sudden joint blockage which often correspond to free intra-articular fragments getting stuck in the joint.
Pain topography
Pains are very often anterior at the front part of the glenohumeral joint and more rarely at the posterior part.
Pain irradiation
Pains will sometimes be projected into the scapula at the posterior part of the shoulder, more rarely at the shoulder stump level or with irradiation into the arm.
Triggering phenomena
Pains can occur during arm elevation movements but often also during external or internal rotation movements.
Note that pains are often weak or even absent at rest with sometimes very significant increase during shoulder mobilization, particularly on reflex gestures.
The importance of pains and correlation with different movements will often depend on osteoarthritis topography, possible presence of osteophytes but also free intra-articular fragments.
Functional impairment
This is the limitation of shoulder joint mobility most often associated with functional use incapacity of the upper limb.
This is the main symptom that will push for consultation and will often be more important and more frequent than painful phenomena.
Most often, the decrease in joint mobility occurs progressively over several months or even several years.
Indeed, due to often moderate pains, there is significant patient adaptation relative to mobility decrease.
Sometimes patients will use the arm on the healthy side to perform activities or use chair/ladder to reach objects at height.
According to osteophyte topography and joint deformation, joint blockages could be either during arm elevation in the air or on rotation movements, particularly to put the hand behind the back or in external rotation.
Evolution therefore often occurs slowly regarding mobility and function loss and pains are fluctuating.
Therefore, patients often present with very advanced osteoarthritis radiological signs.
Shoulder osteoarthritis is therefore often well tolerated for a long time.
The causes of omarthrosis are multiple and often multifactorial but the most frequent are the following:
- Repeated microtrauma: heavy work, contact sports…
- More or less old trauma
- Articular fractures: fracture of the glenoid of the scapula or fracture of the humeral head
- History of shoulder surgery particularly open surgery
- Osteonecrosis of the humeral head: context of alcoholism, long-term cortisone treatment…
- Old rotator cuff rupture: shoulder decentering…
- Shoulder instability with recurrent dislocations
Clinical examination
The clinical examination will mainly find mobility loss with decreased joint amplitudes.
There is no direct correlation between osteoarthritis importance (joint deformation) and function loss importance.
There is no specific clinical test demonstrating glenohumeral joint osteoarthritis.
However, it will be important to perform testing of the rotator cuff tendons of the affected shoulder.
Rotator cuff assessment will be part of the preoperative assessment if surgical intervention is considered later.
(cf. rotator cuff lesion)
Paraclinical and complementary examinations
Standard X-ray: frontal, profile, internal/external rotation
It will provide a large part of the necessary information to assess shoulder osteoarthritis:
- Joint space narrowing (between the humeral head and the glenoid of the scapula)
- Subchondral bone condensation
- Osteophytes (inferior, anterior, posterior…) - great interest of internal/external rotation views
- Humeral head shape (flattening, sphericity loss…)
- Geodes, intraosseous lacunae
- Humeral head centering (eccentricity with elevation would be in favor of associated rotator cuff lesion)
- Bone stock evaluation (especially on the glenoid of the scapula)
Shoulder ultrasound (US)
This is a minimally invasive examination allowing exploration of tendon and muscle structures of the shoulder.
This examination being very operator dependent, it has relatively low diagnostic reliability.
Ultrasound has relatively little interest in the context of shoulder osteoarthritis in terms of diagnosis since it essentially evaluates soft tissues and very poorly bone or articular surfaces.
It will allow evaluation of rotator cuff condition looking for a more or less old and retracted tendon lesion.
Arthro-CT or arthro-MRI (most complete examination)
During this examination, a contrast agent injection is performed in the shoulder joint (between the humeral head and the scapula), followed by a CT scan or MRI.
Contrast agent distribution in the joint will allow perfect visualization of the different rotator cuff tendons as well as bone, cartilaginous and ligament structures.
This is the reference examination to assess shoulder osteoarthritis and possible associated lesions.
It will allow detection of chondropathy lesions at little advanced stages but also polar wear lesions, particularly posterior or anterior, which would not be seen on standard X-rays.
It will estimate much more reliably possible humeral head deformation.
Bone stock assessment, particularly at the glenoid of the scapula and humeral head level (essential element before articular prosthesis implantation).
Evaluation of rotator cuff tendons with in case of rupture estimation of muscle atrophy, amyotrophy and retraction importance…
Staging of chondropathy degree (stage I to IV) and possible osteoarthritis.
It will depend initially on the importance of painful phenomena and priority will be given to treating the different symptoms (symptomatic treatment).
Secondly, physiotherapy will be fundamental to reduce functional impairment and regain maximum autonomy.
Drug treatment
- Level 1 or 2 analgesics (rarely level 3): Treatment choice will depend mainly on pain intensity but also on tolerance to different analgesics (paracetamol, tramadol, codeine…)
- Non-steroidal anti-inflammatory drugs: Treatment to be implemented for 5 to 10 days, combined or not with gastric protectors (PPI). Avoid prolonged treatment with anti-inflammatory drugs.
Immobilization
Shoulder immobilization is done by orthopedic vest also called elbow-to-body splint.
This immobilization will only be done in case of very intense or poorly controlled pain by the different analgesics and should be avoided as much as possible.
In practice, this immobilization will essentially be done in the context of osteoarthritis flare-ups which are sometimes very painful.
The duration of immobilization will be as short as possible to avoid increasing ankylosis and possible joint stiffness.
Cryotherapy
Cryotherapy or icing corresponds to the application of cold in contact with the painful area several times daily.
It will have both an analgesic but also anti-inflammatory role to fight against osteoarthritis flare-ups.
It can be done at home with devices sold in pharmacies or more simply with bags of frozen peas (thus taking the shape of the shoulder).
In case of osteoarthritis flare-up, it is recommended to apply icing at least 4 to 5 times a day.
Cortisone infiltration
It corresponds to an injection of cortisone into the glenohumeral joint in contact with bone surfaces.
Ideally, this cortisone infiltration will be performed under fluoroscopic control with arthrography to ensure proper needle positioning before product injection.
It is important to mention that this infiltration treats the symptoms and repercussions of osteoarthritis but in no case its cause.
Infiltration can have very good efficacy on painful phenomena but also inflammatory in case of osteoarthritis flare-up.
It will be especially effective in case of early and little advanced osteoarthritis allowing functional recovery and improvement of joint amplitudes.
However, in case of advanced osteoarthritis with joint deformation, functional results will be less obvious.
Treatment choice is made on a case-by-case basis and will depend on many clinical and paraclinical factors.
Symptom evolution duration, clinical manifestation importance, response to previously undertaken treatments but also lesions visualized on imaging assessment are all factors that will help us in therapeutic choice.
Pains and functional impairment will be fundamental elements since they cause direct impact on daily life: autonomy decrease, need for help for daily life gestures…
Surgical indications
Surgical treatment in the context of shoulder osteoarthritis consists of articular prosthesis implantation. The principle of this surgical intervention is to replace damaged bone and cartilaginous structures with prosthetic implants fixed in the bone.
When to perform surgical intervention?
- In case of persistent pains not relieved by different conservative treatments (analgesics, physiotherapy, infiltration…)
- In case of functional discomfort, joint blockage and autonomy loss (use of the concerned arm)
There are two main types of shoulder articular prosthesis aiming to restore joint function and mobility.
So-called anatomical prostheses will preserve shoulder physiological anatomy with a convex prosthetic piece at the humeral head level and a concave piece at the glenoid of the scapula level.
Conversely, so-called reverse prostheses modify physiological anatomy with placement of a concave prosthetic piece at the humeral head level and a convex piece at the glenoid of the scapula level.
Prosthesis type choice (anatomical/reverse) will be made according to preoperative assessment (arthro-CT or arthro-MRI), will depend on multiple factors including associated rotator cuff lesions, joint deformation importance particularly of the glenoid of the scapula, possible joint subluxations…
Computer-assisted preoperative planning will help optimal prosthetic implant placement for the best possible functional result.
For more details on the surgical intervention, see the Shoulder Prostheses page.
The role of physiotherapy in the context of shoulder osteoarthritis is the reduction of painful phenomena and the recovery of joint function and use of the upper limb.
Acute phase (osteoarthritis flare-up)
- Massage: muscle relaxation to avoid reactive contractures
- Cryotherapy: analgesic and anti-inflammatory effect
- Gentle mobilization: decoaptation, relaxation and stretching
- Acupuncture, shock waves, mesotherapy…
Chronic phase
- Fight against shoulder elevation and anterior positioning
- Fight against muscle contractures
- Recovery of joint amplitudes
- Muscle synchronization for harmonious movement
After surgical intervention
Physiotherapy is fundamental after shoulder prosthesis implantation. It progressively adapts to healing (4 to 6 months minimum).
Detailed program: Physiotherapy for Shoulder Arthritis.
Like any surgical intervention, the implantation of an anatomical or reverse shoulder prosthesis may carry risks of complications during or after surgery.
The most common risks are:
- Risk of infection
- Bleeding
- Prosthesis loosening
- Nerve damage
- Algodystrophy or inflammatory phenomena
All precautions are implemented to minimize these risks throughout the surgical process (strict asepsis, careful hemostasis, perioperative antibiotherapy…)