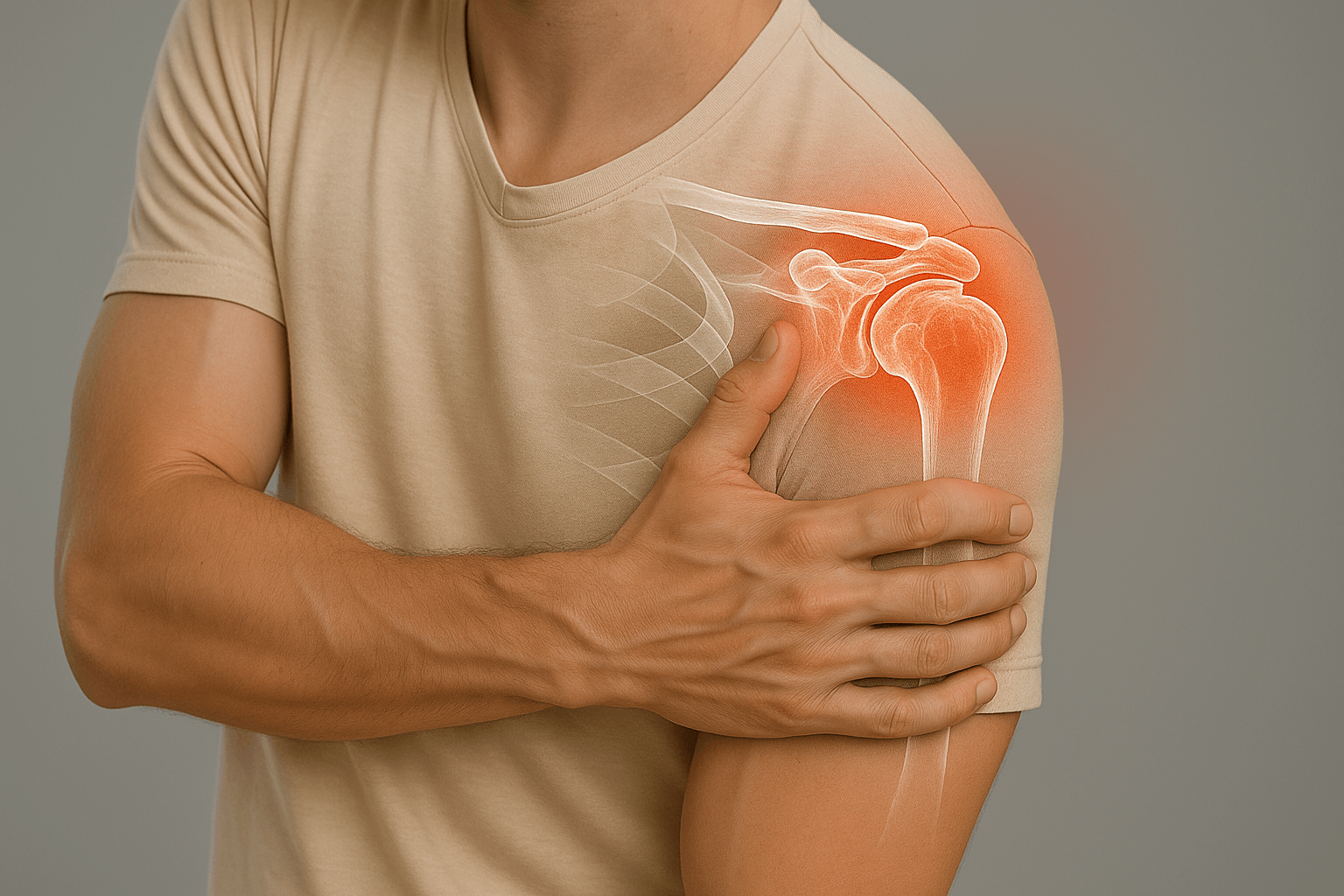
Shoulder Instability
Shoulder instability corresponds to episodes of dislocations or subluxations, often after initial trauma or in hyperlaxity context. This pathology requires specialized management to optimize stability and function.

What is shoulder instability?
Shoulder instability corresponds to episodes of dislocations or subluxations, often after initial trauma or in hyperlaxity context. This pathology can become chronic with apprehension, pain and significant functional discomfort.
The shoulder is the most mobile joint in the human body, making it particularly vulnerable to instabilities. Management depends on instability type, patient age and functional expectations.
Types of instability
Anterior instability
The most frequent, corresponds to forward dislocation of the humeral head. Often related to trauma with Bankart lesion.
Posterior instability
Rarer, corresponds to backward dislocation. Often related to electrical trauma or epileptic seizures.
Multidirectional instability
Instability in several directions, often related to constitutional hyperlaxity or repeated microtrauma.
Mechanisms and causes

Traumatic instability
Initial dislocation after trauma with Bankart lesion (glenoid labrum detachment). Recurrences are frequent in young and athletic subjects.
Associated lesions: Glenoid bone loss, Hill-Sachs notch on humeral head.

Atraumatic instability
Instability related to constitutional or acquired hyperlaxity, often bilateral. Repeated microtrauma may worsen instability.
Favoring factors: Constitutional hyperlaxity, throwing sports, repetitive work above the head.
Symptoms and manifestations

Pain and apprehension
Chronic shoulder pain, apprehension sensation during elevation and external rotation movements. Patient avoids certain movements for fear of dislocation.
Characteristics: Often diffuse pain, aggravated by sports or professional activities.

Dislocation sensations
Sensations of dislocation or subluxation during elevation and rotation movements. Patient may sometimes reduce subluxation himself.
Functional impact: Limitation of sports and professional activities, loss of confidence in the shoulder.
Diagnosis and evaluation
Clinical examination
- Instability tests: Apprehension test, relocation test, sulcus test
- Laxity assessment: Anterior and posterior translation tests
- Neurological examination: Search for associated nerve lesions
- Functional assessment: Impact on daily and sports activities
Imaging examinations

X-rays
Basic examination to assess humeral head position and look for bone lesions

MRI
Reference examination to assess soft tissue lesions and glenoid labrum

Arthro-CT
Specialized examination to precisely assess labrum lesions and plan surgical treatment
Therapeutic options
Post-operative rehabilitation

Rehabilitation after shoulder instability surgery is crucial to optimize functional recovery and prevent recurrences.
Phase 1: Immobilization (2-3 weeks)
Sling according to procedure performed, early passive mobilizations to maintain mobility
Phase 2: Active mobilization (3-6 weeks)
Progressive active mobilizations, beginning of stabilizing muscle strengthening
Phase 3: Strengthening (6 weeks - 6 months)
Progressive strengthening, return to sports activities according to protocol
Return times: Return to contact/throwing sports: 3-6 months according to protocol and evolution.
Possible complications
Instability recurrence
Joint stiffness
Residual pain
Cartilage lesions
Non-consolidation (Latarjet)
Nerve irritation
Practical information
Hospitalization
Outpatient
Anesthesia
General
Immobilization
Sling 2-3 weeks
Physiotherapy
3-6 months
Return to sport
3-6 months