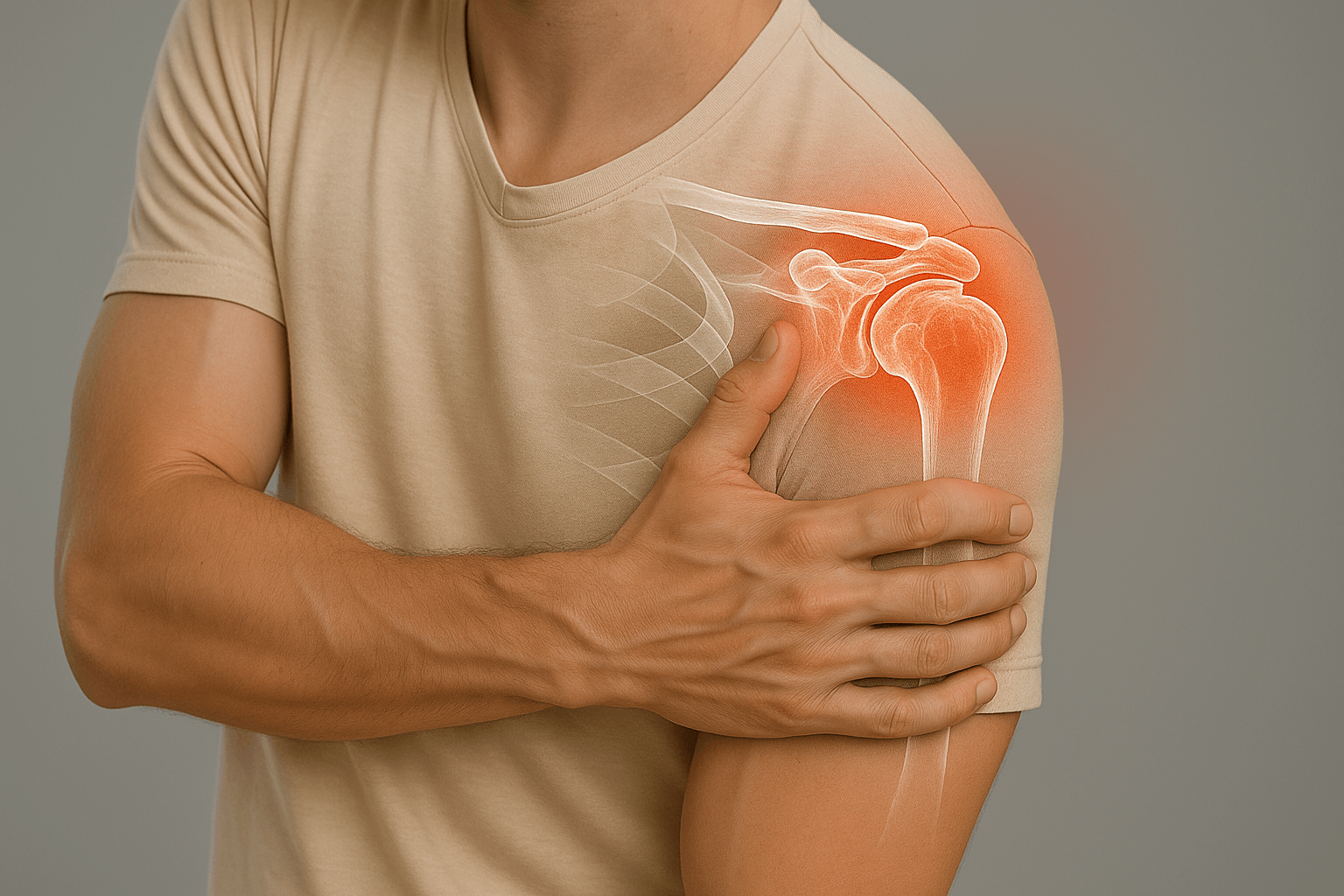
Subacromial Impingement
Subacromial impingement corresponds to excessive and abnormal friction between the rotator cuff tendons and the acromion. This frequent pathology requires specialized management to avoid evolution towards tendon lesions.
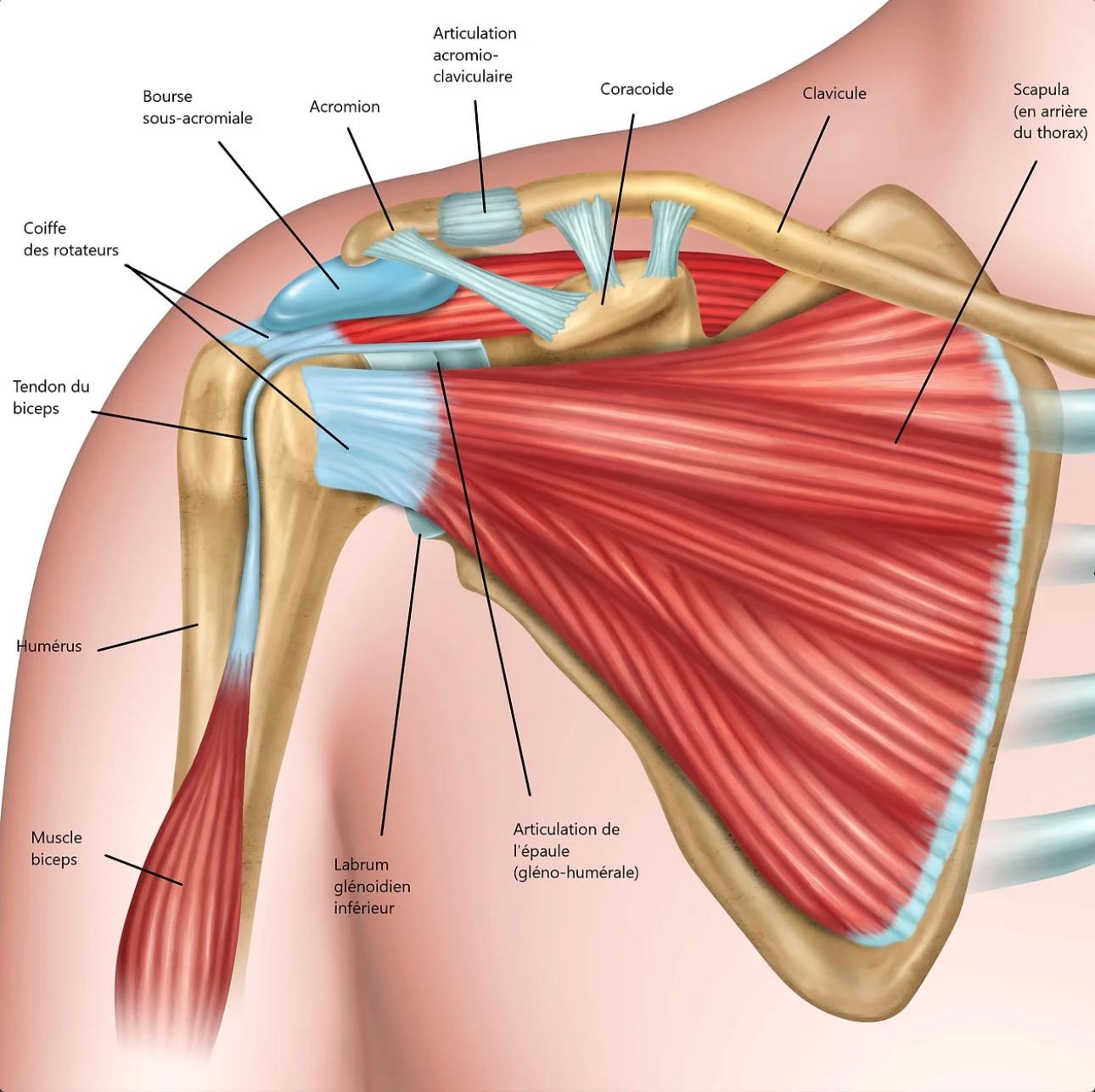
Definition: Subacromial impingement corresponds to excessive and abnormal friction between the rotator cuff tendons and the acromion (acromial bone).
By extension, friction can also occur with the outer quarter of the clavicle or the coraco-acromial ligament located in the extension of the acromion.
The manifestations of this subacromial impingement most often occur during anterior or lateral arm elevation movements.
Physiology
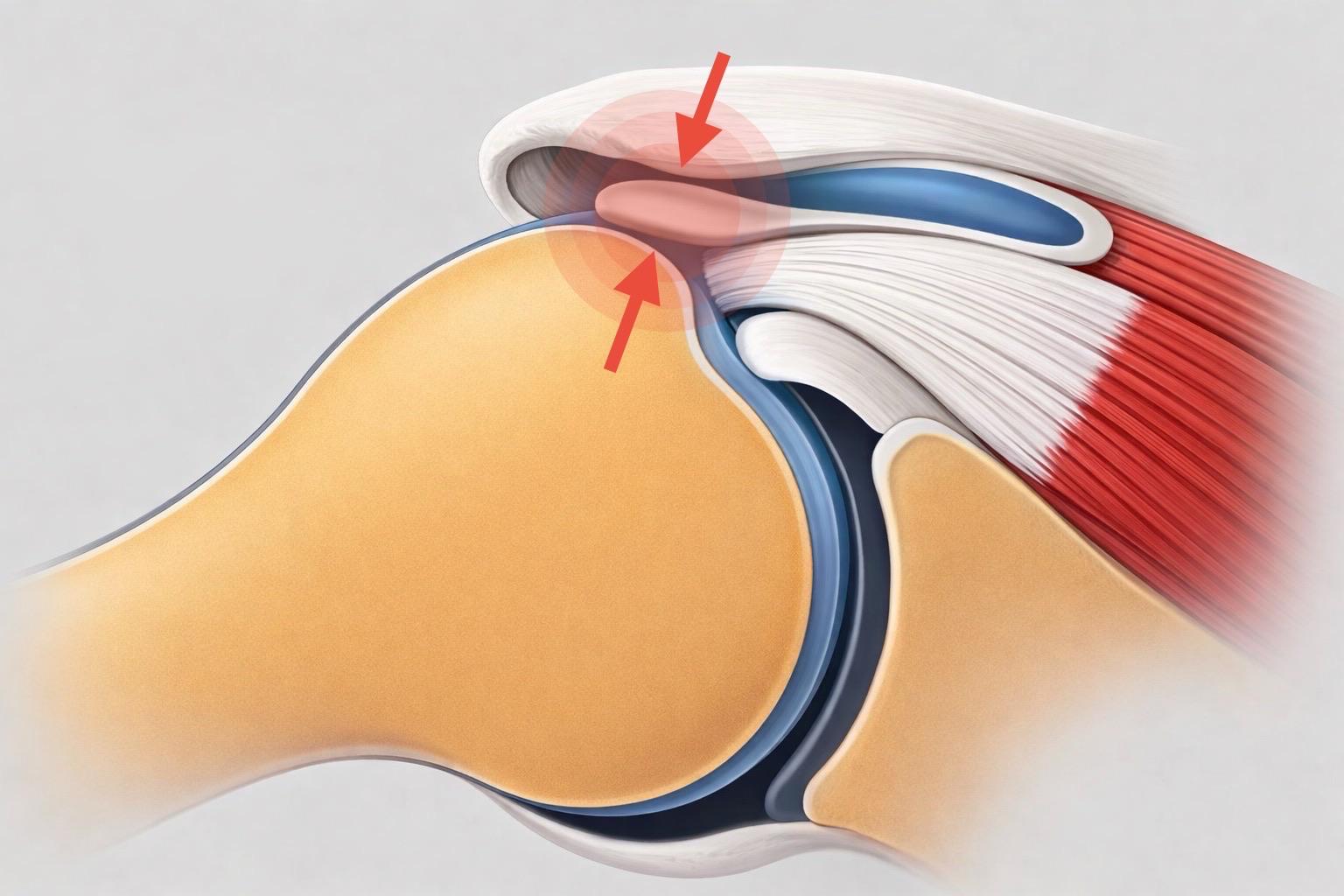
During the physiological movement of arm elevation, the humeral head as well as the different rotator cuff tendons slide harmoniously under the acromial "vault".
This harmonious sliding is made possible thanks to the coordination and balance of the different shoulder muscles.
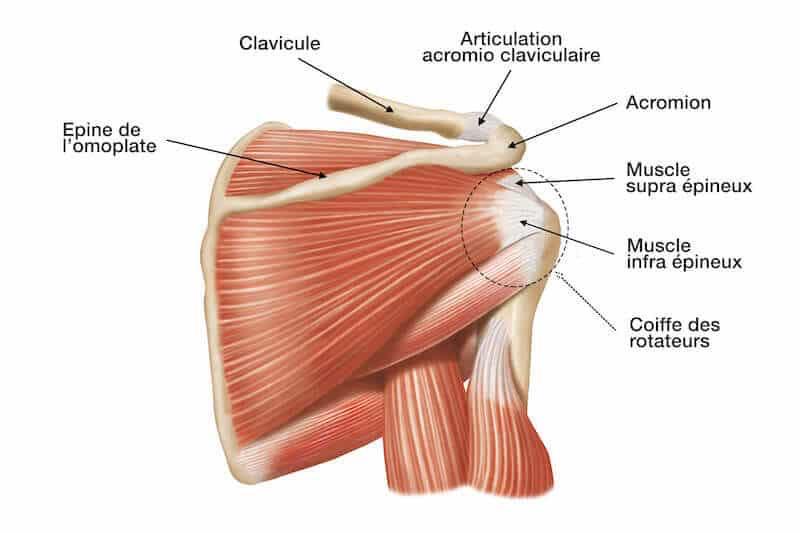
In case of muscular deficiency (abnormality of the balance between muscles) or abnormality at the level of bony structures (hooked or aggressive acromial bone), friction will occur between the bone and the tendons, thus creating the syndrome or subacromial impingement.
Chronic or repeated irritation and friction of the tendons within the subacromial space can lead to tendon lesions (rotator cuff lesion) or bursitis phenomena (inflammation of the subacromial bursa).
There are 2 types of subacromial impingement at the origin of this abnormal friction: subacromial impingement of bony origin (or primary conflict) and subacromial impingement of muscular origin (or induced conflict).
Bony Conflict
In this case, it is the shape of the subacromial vault (aggressive) that will directly come to rub against the rotator cuff tendons.
The shape of the acromial bone is classified into three categories (1, 2 or 3), type I acromion corresponding to a flat acromion, type 2 to a curved acromion and type 3 to a hooked acromion.
It is type II and III acromions that will have the highest risk of creating subacromial impingement.
Secondary or Acquired Conflict
In this case, subacromial impingement comes from muscular deficiency. There is a desynchronization of the different shoulder muscles, preventing normal mobilization and physiological sliding between tendons and subacromial bone (regardless of the shape of the acromion 1, 2 or 3).
Most often there is an anterior displacement as well as an elevation of the shoulder within the joint.
It is this decentering and imbalance of the shoulder that will be responsible for subacromial impingement.
The origin of this muscular deficit can be very diverse, sometimes simply following a fall or shoulder contusion. Sometimes prolonged or intensive activities with arms in the air.
Repeated friction of the acromial bone against the different rotator cuff tendons will cause irritative and inflammatory phenomena (bursitis, tendinitis) and sometimes in case of prolonged evolution, rotator cuff tendon lesions.
These different irritative phenomena explain the clinical manifestations.
Pain
Pain is the main symptom of subacromial impingement. It is most often inflammatory pain, which will be nocturnal and may cause insomnia.
Pain may also cause nocturnal awakenings especially when turning on the affected shoulder.
Sometimes pain is rather morning with unlocking phenomenon allowing a decrease in pain (but pain most often resumes in the evening when activities stop).
Pain characteristics
Topography
Pain is most often located at the shoulder stump or at the anterior part of the acromion.
At the beginning, it is often possible to locate pain at a precise point, then pain tends to diffuse and generalize to the entire shoulder (inflammation).
Pain often tends to diffuse along the deltoid muscle, on the lateral part of the shoulder.
Irradiation
Pain very often tends to diffuse and irradiate at distance.
Irradiation regularly occurs on the external side of the arm and can cause pain up to the elbow and sometimes in the wrist.
Sometimes patients will describe sensations of compression or circular tightening under the deltoid muscle, while sometimes diffuse pain will be along the long head of the biceps.
Conversely, pain will sometimes be ascending with diffusion along the trapezius muscle and sometimes up to the cervical area.
Triggering phenomena
It is the arm elevation movements that will stimulate or trigger painful phenomena. These movements can be in anterior elevation or lateral elevation and pain most often occurs from 80° or 90° (arm horizontal) with often sensation of catching or audible cracking.
Consequences of pain
Functional impairment
Functional impairment corresponds to an inability to normally mobilize the affected limb. In the context of subacromial impingement, it is most often a functional discomfort rather than true impairment.
In case of subacromial impingement, there may be inconsistently and more or less importantly, discomfort or inability to mobilize the arm and shoulder.
A temporary and transient picture of paralyzed shoulder or "dead arm" may also appear, with total inability to actively mobilize the shoulder. This situation most often occurs after prolonged or repeated activity with the arm in the air and is accompanied by intense pain.
After a few hours or days, arm use returns progressively.
In case of prolonged functional impairment or inability to actively mobilize, possible rotator cuff lesions or capsulitis retractile lesions should be considered.
Lack of strength: In some cases, functional impairment will manifest as a lack of strength corresponding to difficulty or impossibility of performing movements against resistance. In particular, it will be difficult or impossible to lift weights or loads in height above shoulder level.
Muscle contractures
Chronic pain at the shoulder level can lead to muscle contracture phenomena at the level of the large muscle groups surrounding the shoulder.
The muscles mainly concerned are the latissimus dorsi muscle, the pectoralis minor but also the trapezius muscle.
Contractures of these large muscle groups can cause vicious positions at the shoulder level. It will typically be a vicious position in shoulder elevation upward as well as a forward displacement of the shoulder.
It is this vicious position that will risk accentuating and maintaining this subacromial impingement. (Painful vicious circle)
Clinical examination
The clinical examination will find signs of subacromial impingement more or less marked.
Several clinical tests will allow to detect signs in favor of subacromial impingement:
- Neer maneuver
- Yocum test
- Hawkins test
- Gerber test
These different tests are more or less specific to subacromial impingement and may be associated with possible rotator cuff deficits in case of lesion.
Sometimes the performance of these clinical tests will not be possible due to often significant painful phenomena, especially during associated bursitis or tendinitis.
Typically, passive shoulder mobilization should be preserved even if active mobilization is limited or painful. Otherwise, capsulitis retractile or another shoulder stiffening phenomenon should be considered and searched for.
Paraclinical and complementary examinations
Standard X-ray: frontal and profile
This is the first routine examination to perform in case of shoulder pain. It will provide much information on the different bony structures of the shoulder.
It will also allow to show many direct or indirect signs that may testify to subacromial impingement.
Frontal X-ray:
- Distance between acromion and humeral head, allows to judge centering or possible elevation of humeral head relative to glenoid (elevation of humeral head in case of rotator cuff rupture)
- Shape of acromion, more or less aggressive character
- Shape of acromioclavicular joint, possible arthropathy and inferior overhang
- Possible intratendinous calcification
- Possible glenohumeral osteoarthritis
Profile X-ray: It allows to visualize the shape of the acromion and classify it according to types 1, 2 or 3.
Attention: an aggressive shape of the acromion on X-ray is not synonymous with subacromial impingement even if it increases its probability.
Standard shoulder X-ray only allows to see bony structures and in no case tendon or ligament structures.
Ultrasound
This is a minimally invasive examination allowing to explore tendon and muscle structures of the shoulder.
This examination being very operator-dependent, it has relatively low diagnostic reliability.
Ultrasound will allow to find signs of tendinitis with rotator cuff tendon thickening or even erosion.
It will also allow to search for signs of subacromial bursitis, namely inflammation of the bursa physiologically present between the acromion and the rotator cuff.
Possible rotator cuff lesions will also be searched for, whether fissure, rupture or detachment.
These rotator cuff lesions are often the consequence of prolonged subacromial impingement or an added fall.
Arthro-MRI or arthro-CT: reference examination
During this examination, a contrast product injection is performed in the shoulder joint (between the humeral head and the scapula), followed by a CT scan or MRI.
The distribution of the contrast product in the joint will allow perfect visualization of the different rotator cuff tendons as well as bony, cartilaginous and ligament structures.
This examination will therefore allow to visualize possible fissure or complete or incomplete rotator cuff rupture, consequence of prolonged subacromial impingement.
Muscle assessment will also be performed with search for possible atrophy or fatty involution of rotator cuff muscles (abnormality in case of old rotator cuff rupture).
It will also be possible to visualize the acromial bone in the different planes of space and notably its aggressive character on the rotator cuff tendons.
The examination will detect possible signs of subacromial bursa inflammation (bursitis) as well as thickening or possible calcification of the coraco-acromial ligament also testifying to subacromial impingement.
Finally, the acromioclavicular joint will also be visible allowing to highlight signs of acromioclavicular arthropathy more or less responsible for underlying tendon conflict.
This paraclinical examination is therefore the reference examination that is the most exhaustive to explore the shoulder joint.
Treatment choice is made case by case and will depend on many clinical and paraclinical factors.
The duration of symptom evolution, the importance of clinical manifestations, the response to different previously undertaken treatments but also the aggressive character of the acromion and/or the coraco-acromial ligament… are elements that will be taken into account in the treatment choice.
Surgical indications
Surgical treatment in the context of subacromial impingement consists of performing an acromioplasty.
This acromioplasty corresponds to decompression of the subacromial space by filing and thinning of the acromial bone at its deep part.
In which cases to consider surgical solution:
- In case of prolonged or recurrent subacromial impingement
- In case of ineffectiveness of well-conducted symptomatic treatment
- In case of ineffectiveness of well-followed physiotherapy
- In case of aggressive character of the acromial vault (acromion, coraco-acromial ligament, aggressive acromioclavicular joint…)
Shoulder acromioplasty
This is a surgical intervention performed under arthroscopy allowing to file and sand the deep part of the acromion.
Shoulder arthroscopy corresponds to the introduction of a camera into the joint and subacromial space to explore and treat different lesions.
The interest of arthroscopy compared to open interventions is the absence of muscle lesion due to the absence of extensive surgical approach but also the much lower risk of infection or hemorrhage and the quasi absence of post-operative scar at distance.
The goal of the intervention is to clean the subacromial space and decompress it. Under arthroscopy, different surgical instruments allow to file and sand the deep face of the acromion but also to release the coraco-acromial ligament often conflictual. It will also be possible to perform partial joint resections notably of the outer quarter of the clavicle in case of acromioclavicular arthropathy.
This decompression is done with 2 or 3 incisions of approximately 1 cm allowing to pass surgical instruments and the camera.
Note: in case of associated lesion of rotator cuff tendons or other ligament lesion, it will be possible in the same operative time to perform repair of these different lesions under arthroscopy.
For more details on the surgical intervention, consult the Shoulder Acromioplasty page.
Physiotherapy has a fundamental role in the background treatment of subacromial impingement, whether pre-operatively or after surgical intervention. The main goal is shoulder recentering work.
For detailed information on the specific physiotherapy and self-physiotherapy program for subacromial impingement, consult the dedicated page: Physiotherapy for Sub-acromial Impingement.
- Impingement = abnormal friction between the acromion and rotator cuff tendons.
- Manifestations = pain and inflammation +/- functional impairment
- Examination = arthro-CT or arthro-MRI
- Treatment =
- If conservative: analgesics and physiotherapy
- If surgical: acromioplasty
- Acromioplasty =
- Under arthroscopy
- Hospitalization 0 to 2 days
- Under general anesthesia
- Immobilization 15 days to one month
- Post-operative physiotherapy 2 to 3 months