Shoulder Calcifications
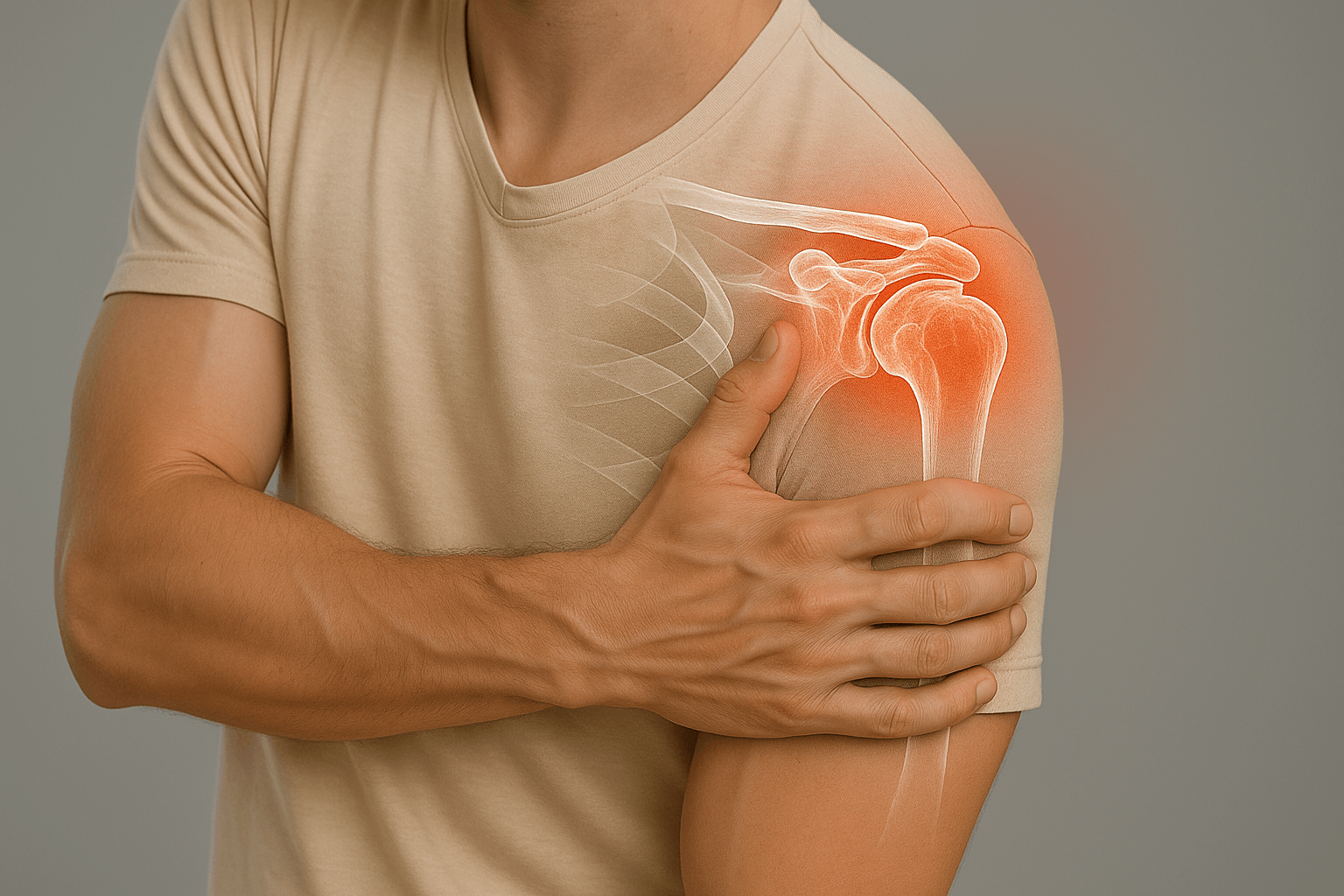
Shoulder calcifications correspond to calcium deposits within tendons, responsible for acute pain and functional limitations. This pathology requires specialized management to optimize comfort and function.

What are shoulder calcifications?
Shoulder calcifications correspond to calcium deposits within tendons, most often the supraspinatus. These deposits are responsible for acute pain and significant functional limitations.
Calcifying tendinopathy evolves by sometimes very intense flares and requires adapted management according to the evolutionary phase and the importance of symptoms.
Natural evolution and phases
Formation phase
Progressive calcium deposit in the tendon, often asymptomatic or slightly painful.
Rest phase
Stabilization of calcium deposits, generally slightly symptomatic.
Resorption phase
Resorption of calcifications, often the most painful phase with inflammatory flares.
Favoring factors

Demographic factors
Typical age of 30-50 years, with female predominance. Calcifications can be bilateral in some cases.
Metabolic terrain: Certain metabolic disorders may favor calcification formation.

Microtrauma
Repeated shoulder stress, professional or sports activities above the head may favor calcification appearance.
Spontaneous regression: Many calcifications regress spontaneously without specific treatment.
Symptoms and manifestations

Pain
Acute pain, sometimes nocturnal, with very intense inflammatory flares. Pain can be disabling and wake up at night.
Characteristics: Often sudden, intense pain, with significant limitation of shoulder mobility.

Functional limitation
Significant limitation of arm elevation, difficulties for daily gestures and professional activities.
Impact: Significant reduction in quality of life and functional performance.
Diagnosis and evaluation
Clinical examination
- Pain on palpation: Localized sensitivity at supraspinatus tendon level
- Mobility limitation: Restriction of elevation and abduction movements
- Specific tests: Rotator cuff tests often positive
Imaging examinations

X-rays
Reference examination to visualize calcifications and assess their size and location

Ultrasound
Minimally invasive examination to assess inflammation and tendon vascularization

MRI
Reference examination in case of diagnostic doubt or for surgical planning
Therapeutic options
Post-operative rehabilitation

Rehabilitation after calcification treatment is essential to optimize functional recovery and prevent recurrences.
Phase 1: Pain control (0-2 weeks)
Pain control, passive and assisted mobilizations to maintain mobility
Phase 2: Range recovery (2-6 weeks)
Progressive recovery of movement ranges and gentle strengthening
Phase 3: Strengthening (2-3 months)
Progressive strengthening and return to overhead gestures
Return times: Progressive sports return after 8-12 weeks depending on evolution.
Possible complications
Transient stiffness
Residual pain
Calcification recurrence
Infection
Hematoma
Nerve lesion
Practical information
Hospitalization
Outpatient
Anesthesia
General
Immobilization
Sling 1-2 weeks
Physiotherapy
8-12 weeks
Return to sport
8-12 weeks