Acromioclavicular Arthropathy
Acromioclavicular arthropathy corresponds to degenerative or post-traumatic involvement of the acromioclavicular joint. This frequent pathology requires specialized management to optimize comfort and function.

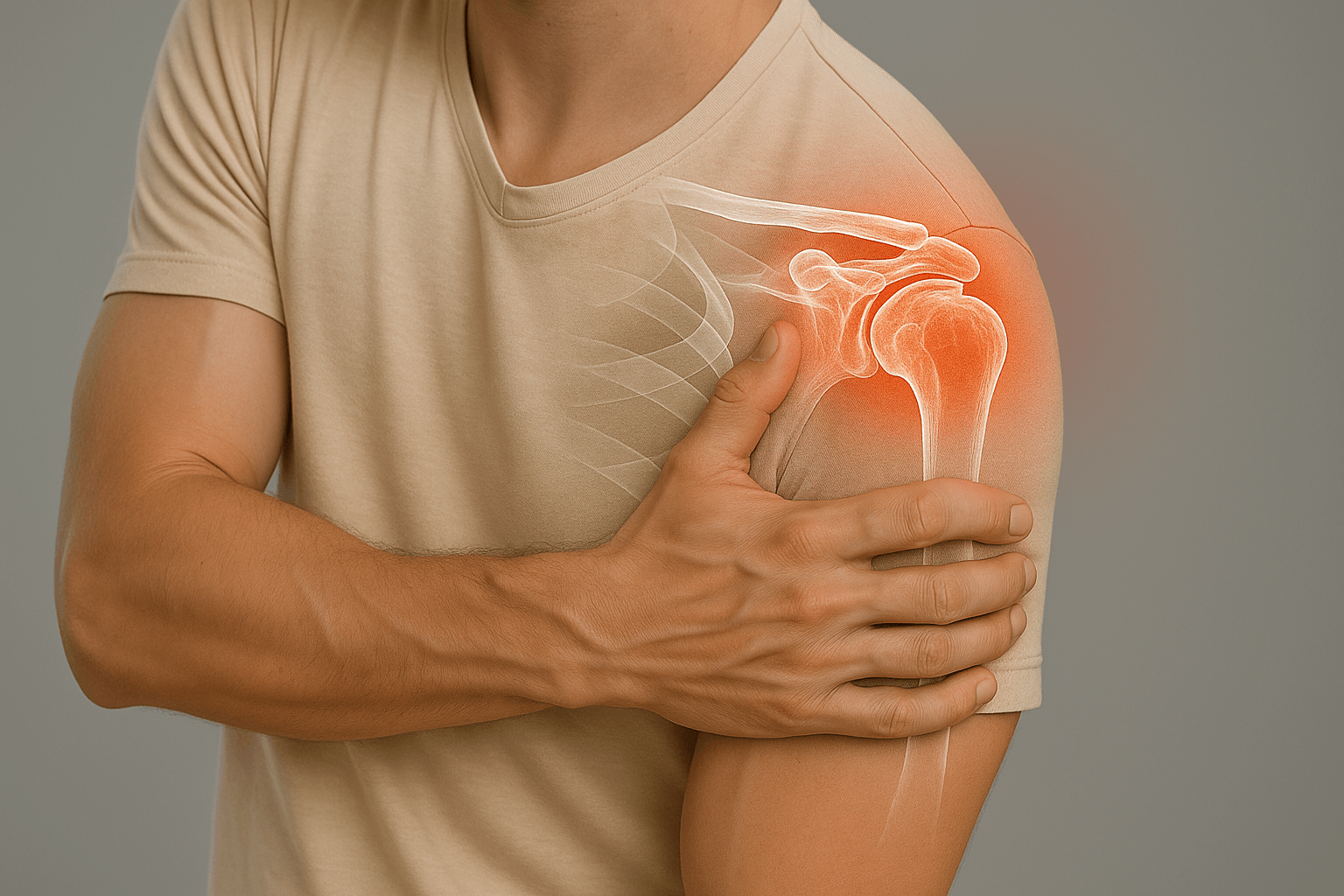
What is acromioclavicular arthropathy?
Acromioclavicular arthropathy corresponds to degenerative or post-traumatic involvement of the acromioclavicular joint, source of localized pain at the top of the shoulder.
Favoring factors include repetitive load activities, age, and possible association with subacromial impingement. This pathology can significantly impact quality of life and professional activities.
Pathophysiology and favoring factors
Degenerative wear
Progressive wear of the AC joint with osteophyte formation and articular cartilage degradation.
Repeated microtrauma
Work or sports above the head, repeated stress on the acromioclavicular joint.
Subacromial impingement
May coexist with subacromial impingement, creating a complex clinical picture.
Symptoms and manifestations

Pain
Pain localized above the shoulder, particularly on palpation of the acromioclavicular joint. Pain may radiate to the trapezius and be aggravated during overhead movements.
Characteristics: Often chronic pain, aggravated by load activities and arm elevation movements.

Functional discomfort
Limitation of overhead movements, difficulties during professional or sports activities requiring arm elevation.
Impact: Reduction in quality of life and performance in daily and professional activities.
Diagnosis and evaluation
Clinical examination
- Palpation: Pain on direct palpation of the AC joint
- Specific tests: Cross-body compression test, horizontal adduction test
- Functional assessment: Limitation of elevation and abduction movements
Imaging examinations

Targeted X-rays
Reference examination showing joint space narrowing, osteophytes and deformations

Ultrasound
Minimally invasive examination to assess inflammation and soft tissue lesions

MRI
Reference examination for complete assessment and surgical planning
Therapeutic options
Post-operative rehabilitation

Rehabilitation after lateral clavicle resection is essential to optimize functional recovery and prevent complications.
Phase 1: Immobilization (1-2 weeks)
Comfort sling, gentle immediate mobilization respecting pain
Phase 2: Active mobilization (2-4 weeks)
Progressive shoulder mobilization in all directions without forcing
Phase 3: Strengthening (4-8 weeks)
Progressive strengthening of shoulder muscles and return to activities
Return times: Manual and sports activities: 6–8 weeks depending on pain and recovery.
Possible complications
Infection
Hematoma
Nerve lesion
Painful recurrence
AC instability
Complex regional pain syndrome
Practical information
Hospitalization
Outpatient
Anesthesia
General
Immobilization
Sling 1-2 weeks
Physiotherapy
6-8 weeks
Return to activities
6-8 weeks